What is lung cancer?
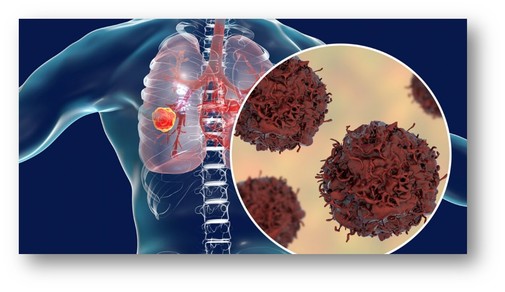
Cancer is a disease in which cells in the body grow out of control. When cancer starts in the lungs, it is called lung cancer.
Lung cancer begins in the lungs and may spread to lymph nodes or other organs in the body, such as the brain. Cancer from other organs also may spread to the lungs. When cancer cells spread from one organ to another, they are called metastases.
To help detect lung cancer and prevent it from spreading, get screened early - find a local lung cancer screening center near you.
Types of Lung Cancer
Lung cancers usually are grouped into two main types called small cell and non-small cell. These types of lung cancer grow differently and are treated differently. Non-small cell lung cancer is more common than small cell lung cancer.
These categories refer to what the cancer cells look like under a microscope. If you have lung cancer (especially non-small cell lung cancer), your doctor may run tests to find out if you have a change in your genes (genetic mutation). The results of these tests help your doctor know which treatments will work best for you.